Endodiabology 2005; Issue 3 (October)
ENDODIABOLOGY
NORTHEAST NEWSLETTER
FOR SPRs AND BOSSES TRAPPED IN THE NORTHERN DEANERY
October 2005
Editors: Shahid Wahid and Petros Perros
Associate Editors: Freda Razvi, Akheel Syed and Ebaa Al-Ozairi
SpR PLACEMENTS (NTN/VTN year of training from 1st October 2005)
RVI- Arun(5), Salman Razvi (3), Akheel Syed (4), Andrew Advani (3/4), Suresh Vaikkakara (visiting SpR)
Freeman- Eelin Lim(3), Reena Thomas (4), Vishmawitra Sharma
North Tyneside/Wansbeck- Muthu Jayapaul (3) /Chandima Idampitiya (1)
South Tyneside- Ibrahim M Ibrahim (4)
Gateshead- Ravi Erukalapati(1)
Sunderland-Isha Malik(1), Subir Ray (2)
North Tees/Hartlepool- Sony Anthony(4)/ Peter Carey(3)
Middlesbrough- Simon Ashwell(5), Sukesh Chandran (2), Asgar Madathil (2)
Carlisle- Khaled Mansur-Dukhan (2)
Bishop Auckland / Durham- Beas Bhatacharya (3)/Jeevan Metayil (1)
NGH/QEH- Yasir Elkhatim
Research with numbers (supervisor)- Latika Sibal (Prof Home), Arutchelvan Vijayaraman (Prof Home), Ravikumar Balasubramanian (Prof Taylor), Ebaa Al-Ozairi (USA-Prof Home)
Acting up David Woods (5)
MEETINGS / LECTURES / ANNOUNCEMENTS
10th-11th October 2005 Controversy or Consensus in the Diabetic Foot Conference, London. Contact SB Communications Group
21ST October 2005 Deadline for BES abstract submission. See www.ece2006.com
25th October 2005 55th Meeting of British Thyroid Association, London. Contact Mark Vanderpump
26th-27th October 2005 ABCD Autumn meeting, London. Contact www.diabetologists.org.uk
26thOctober 2005 Northern Endocrine & Diabetes Autumn CME,James Cook University Hospital. Contact Simon Ashwell .
3rd November 2005 RCP Update in Medicine, Freeman Hospital. Contact Lorraine Waugh
7th-9th November 2005 196th Meeting of the Society for Endocrinology, London. Contact www.endocrinology.org
9th November 2005 North East Obesity Forum, Freeman Hospital 1600-1800, “the Liver in Obesity”. Contact Karen Blackburn or Nigel Unwin
12th November 2005 Association of Physicians meeting,South Tyneside District Hospital. Contact Roy Taylor .
14th November 2005 Regional Neuroendocrine Tumour Meeting, Freeman Hospital 1730-2030, Contact Beverley Ashton
14th-16th November 2005 3rd National MED REG conference, London. Contact www.mahealthcareevents.co.uk or Mark Allen Group
25th November 2005 Abstract Deadline for DUK APC Birmingham March 2006.
30th November 2005 Northern Endocrine Regional Research and Audit Group (NERRAG) meeting, Lumley Castle, Chester-le-street, Durham. Contact Shahid Wahid
14th December 2005 GIM training ½ day-Freeman Hospital. Contact Lorraine Waugh 0191 223 1247 Lorraine Waugh
15th December 2005 SpR Assessment methods training workshop, James Cook University Hospital 1230-1700. Contact Helen Scales
15th February 2006 Society for Endocrinology Clinical Cases meeting, London. Contact Ann Lloyd
TRAINING ISSUES
Registering with JCHMT/PMETB It is essential that all new SpRs (even LATs) register with the PMETB (used to be JCHMT). Not doing so means your training is not counted and you cannot have a RITA.
SpR Feedback Recently feedback forms for training posts have been circulated to all SpRs. Please complete one form for each training post you have been to in the region as an SpR and return electronically to Shaz Wahid. The results for each individual unit will be sent to them along with a regional summary for comparison. This will allow individual units to improve training. The summary results and examples of practice will be discussed at the annual Trainers meeting. The process will be completed every 3-yrs (to coincide with planned Programme Director change over) so to maintain SpR anonymity.
SpR Database The STC are building an updated database of trainees. Could all SpRs with a number forward their NTN details and CCT date ASAP to Shaz Wahid.
Log Book/Portfolio Documentation It is a trainees responsibility to make sure their portfolio/log book is prospectively completed and the necessary signatures obtained. Any experience that is not signed off by your educational supervisor at the time cannot be counted towards training.
The Run Through Grade-An update from Shaz Wahid and John Parr As of August 2007 all SHO posts in the region “will” join the PIMD school of medicine, with Basic Specialist Training in Medicine provided in 2-year rotations based around 4 geographical areas with associated hospitals: Wearside (Sunderland Royal, South Tyneside); Newcastle (FRH, FRH, QEH, Northumbria); Durham (UHND, Bishop Auckland, Darlington); Teeside (JCUH, Friaridge, North Tees, Hartlepool). The rotations will be governed by the PIMD. Although floated in a discussion document initially, at a recent GIM STC meeting Nancy Redfern has confirmed that the deanery will be adapting this model. A lot of groundwork is required (an understatement) and the following preliminary timetable was sketched out for our region:
1. By Jan 06
All the "Ology" Specialty programme directors/committees will be consulted and asked what they want of the BST programme for people acceptable to their specialty training programmes, and how do they want to be represented; this will also include the likes of Radiology where medical SHOs also currently go to (the current estimate is that only 40% SHOs go onto medical specialty training programmes so other routes of specialization also need to be catered for in a Basic Medical Specialty Training Programme.
How many non-F2 SHOs (approved posts; Trust doctors; Clinical Fellows etc) do we have in the region?
What posts do we have within the "obvious base units" and are there enough posts to provide suitable rotations?
Who will be the local Trust doctor charged with doing the donkey work within each Trust?
Workforce Planning issues to be sorted out with SHA.
2. By March 06
A draft working plan/document to be produced and presented.
Trusts' Managers to be approached formally.
Final document/plan to be agreed.
3. Between April and Dec 06.
Appoint Programme Directors;
Produce Rotation Specifications; Means of Assessment etc
Assess individual posts to ensure they can provide what the rotations need - (?Trainers may need to produce their own portfolio!).
Means of appointment (?National or Regional); Employment issues - e.g. Trust or Regional Contracts etc.
4. Feb 07
Advertise Posts for appointment for 1st August 2007
There are many outstanding issues which the PIMD will need to take on board; for example;
a) Role of current Royal College approval visits
b) Role of MRCP if the SHOs get their CCST in Acute Medicine at the end of the 2 year BST programme (the inference here is they may even be eligible as a Consultant in Acute Medicine after only 4 years training!).
c) What becomes of the "slow" trainee - will a 3rd year be needed?
d) How will the needs of Radiology, Dermatology, Anaesthesia etc be accommodated within the BST programme.
The STC is considering the implications of the above for our Training Programme. The PIMD are already setting up work-shops to prepare STCs for the Run through grade
Academic SpR rotation The STC are developing a post for an SpR to fill who is academically inclined. The details are still embryonic, but the attributes of future applicants should be:
-Wants an academic (eg. University, not NHS) career
-Already has a good first research degree (MD/PhD)
-Has already a significant publication record (eg. 4 rated papers for
the purposes of research assessment exercise [IF>5], or close to this)
-Has clear and independent research plans that will lead to an
application for a Clinician-scientist fellowship post within 12 months
of starting
-Has strong backing both from an Academic supervisor and a second
Clinical supervisor
-Has already been successful in obtaining some independent research
grant support
Obviously this is a tall order, and the post won't always be filled. An Academic SpR post will be a significantly different experience to a regular SpR post and not just a bland alternate designation with the same training expectations and experiences. Watch this space!
Community Diabetes Training/exposure in this area should consist of the following:
-Attendance at GP diabetes Clinics in the community to view process of care
-Participation in educational activities involving primary care health professionals
-Interaction with local Diabetes UK patient groups
-Attendance at a Diabetes Clinical Network or other management activity involving primary and secondary care interaction
-Participation with Diabetes Specialist Nurses in the community, e.g. home visit
Evidence may comprise reflective accounts, case based discussions, minutes of meetings, programme of events or feedback forms. These are the minimum training standards. Trainees keen to pursue a career in Community Diabetes will need a different slant to their rotation (cv academic rotation), which will require more extensive exposure to community diabetes and SOLID management training. The STC may have to look at this issue in due course.
SpR adverts for NTNs/LATs New PIMD regulations mean that each specialty will be allowed only 2 advertisements per year for Numbers/LAT appointments. The adverts for DM/Endo will be scheduled for end of September (this year 24th September) and Middle of April (next year 14th April). We therefore will only have 2 appointment panels per year for SpRs with a limited window. This has major implications:
1. All SpRs wishing to undertake an out of programme experience (formal research/travel abroad/acting up) or leave the rotation in 2006 are to give Shaz Wahid notice of the exact dates of absence(in writing) by the 1st March 2006. This will then allow the appropriate advertisement to be placed in April 2006 with an appointments panel convened in May/June 2006. Be warned that once SpRs have gave formal notice and the interviews have taken place with a replacement appointed for the period of absence from the rotation there is no going back. Any SpR missing this deadline will not be allowed to come off the rotation until the next appointments panel in October/November 2006 can appoint a replacement.
2. For SpRs with CCSTs due in 2006, the appointments panel in May/June 2006 will automatically appoint a replacement to start 6-months after their CCST date. This may be sooner, if the CCST holder accrues a post earlier than their 6-month grace and enough notice has been given to the appointments panel.
Inevitably a gap may arise in the rotation. The PIMD will post an advert for a LAS that does not require an appointments panel.
New Assessment tools Please see the following website. As of October 2005 Multisource feedback (MSF) and Directly Observed Procedural Skills (DOPS) will be formally introduced and Mini Clinical Evaluation Exercise (Mini-CEX) will go live from October 2006. Also read Ebaa’s excellent thought provoking letter below.
Training Committee Committee Chair- Jola Weaver; Regional Speciality Advisor- Richard Quinton; Programme Director- Shahid Wahid; Consultant member- Jean Macleod; Consultant member (Research Advisor)-Simon Pearce; Consultant member- Simon Eaton; Consultant member- Ronan Canavan; SpR representative- Simon Ashwell; SpR representative- Andrew Advani.
NEW FACES ON THE SCENE
Welcome to Chandima Idampitiya. She joins us as a new NTN beginning at Northumbria.
Welcome to Suresh Vaikkakara. He is a visiting SpR from India based at the RVI.
OLD FACES ON THE GO
Congratulations to Kamal Abouglila on appointment to the post of Consultant in Diabetes and Endocrinology at University Hospital of North Durham.
NEWS FROM THE NORTHEAST
Congratulations to Jeevan Matayil and Ravi Erukulapati on their NTNs.
Congratulations to Richard Quinton and Family on the birth of Baby Oliver.
Congratulations to Akheel Syed and family on the birth of baby boy sunain.
The Programme Director Change has been brought forward, with Shaz Wahid taking over from Richard Quinton on 1st October 2005.
LETTERS
Contributions for this section can include meeting reports, research experiences, book reviews, experiences abroad, and anything else you feel may benefit trainees and trainers around the region. The success of this section really does depend on YOU.
The Death of General Medicine as a dual speciality is nigh
Shaz Wahid
Some may think I am mad, but throughout my training as both an SpR and SHO I thoroughly enjoyed GIM in both its acute medicine and out-patient varieties. My career choices have been coloured by Physicians such as David Carr, Rudy Bilous and Jean MacLeod to name but a few who have (had) established GIM out-patient clinics when I was on their team. This exposure I believe has contributed to my development. It was with a heavy heart that I have recently had to stop taking GIM out-patient referrals from GP colleagues and now run a mainly endocrine clinic with a spattering of ward follow-up patients. The reason for this is the ever-increasing specialist work-load and pressures such as choose and book to name a few. Once Acute Medicine becomes an entrenched speciality and there are enough Acute Physicians, even the acute medicine will disappear into the horizon and I will probably be writing a similar piece in ENDODIABOLOGY. What does this trend hold for future training programmes? I believe that the writing is on the wall for dual speciality training between GIM and DM&Endo. When this may occur is any ones guess, but the split may well be traumatic.
RCP Assessment Tools: Grading the Graders- The missing link!!!
Ebaa Al-ozairi
Assessment is an essential element of all educational systems and to be useful it must be viewed as an integral rather than series of events. Royal College of Physicians (RCP) has recently released new assessment tools for SpRs. Many of the tools have been widely used in the USA and Canada; however can they be applied to the UK system???? In my one year of experience in the USA at Harvard with the remodelling of postgraduate training in the UK has fuelled me to explore discrepancy in the training system and the impact towards a better training system
With the development of modernizing medical careers, it has come to my attention that the onus is on the trainee themselves including evaluation, continuing assessment and examination with huge issue not being addressed: GRADING THE GRADERS- The missing link!!!!!
Mini-Cex: While this method is certainly widely used in USA for the medical students it is hardly used at the fellow stages (equivalent to the SpR stage). Both the American Board of Internal medicine and the fellowship exams are solely based on MCQ with no clinical components. In Canada twice a year mini-cex evaluation takes place in the residency program to prepare the interns for the clinical component of internal medicine exams. Both USA and Canadian systems do not allow interns or fellows to see any in-patient consultation or outpatient without individual discussion of the plan in the presence of the attending (Consultant) who needs to see every single case both at the inpatient and the Outpatient and this is regarded as continuing educational process and mimic the Mini Cex for the later stages. This certainly can not be applied to UK training due to the number of patients seen.
MSF and Raters: I strongly believe in team work and the concept is very appealing. However this method may be useful as an assessment tool after foundation year and may be in the initial stages of higher training but certainly neither in the last 2 years when SpR should be looked at as a senior figure nor at foundation year 1 (F1). Why should doctors get assessed by the allied health professional when they are not assessed by SpR and junior doctors???? Junior doctors in the UK are under so much pressure by the nursing staff and in my opinion the majority of the house officers have enough stress at this stage.
In both the USA and the Canadian system an essential part of the assessment is the complete evaluation of the residents and fellows by their staff (consultant). This is a detailed evaluation of availability, patient care, teaching, communication skills and system based practice. I strongly believe this is a powerful tool that has been missed out at the postgraduate stage although it is widely emphasized in the UK undergraduate system
Similarly the attending evaluates the residents/fellow however it is the duty of the of the attending to take the lead in arranging the evaluation dates and discussing all the evaluations with the resident/fellow rather than resident/fellow running around making appointments.
I strongly believe in assessment as a tool to validate educational effort. Without adequate summative assessment we can not fulfil our obligation to society to assure physicians training meets the higher state of knowledge, competence and professionalism. The UK has been well known for the quality of trained physicians but the time came to polish up to excellence level.
RECENT PUBLICATIONS FROM THE NORTHEAST
Please send us your recent publication for inclusion in the next newsletter.
1. Brook, Clayton and Brown: Clinical Paediatric Endocrinology (5e), which will be launched this month at the European Society of Paediatric Endocrinology meeting with a chapter "Polyglandular Syndromes" by Owen CJ, Cheetham TD and Pearce SH.
2. Carey PE, Gerrard J, Cline GW, Dalla Man C, English PT, Firbank MJ, Cobelli C, Taylor R. ACUTE INHIBITION OF LIPOLYSIS DOES NOT AFFECT POST-PRANDIAL SUPPRESSION OFENDOGENOUS GLUCOSE PRODUCTION. Am J Physiol Endocrinol Metab. 2005 Jul 5; [Epub ahead of print]
3. Hart RH, Kendall-Taylor P, Crombie A, Perros P. Early response to intravenous glucocorticoids for severe thyroid-associated ophthalmopathy predicts treatment outcome. J Ocul Pharmacol Ther. 2005 Aug;21(4):328-36.
4. Home PD, Home EM. International textbook of diabetes mellitus. Diabet Med. 2005 Oct;22(10):1460.
5. Home PD, Hallgren P, Usadel KH, Sane T, Faber J, Grill V, Friberg HH. Pre-meal insulin aspart compared with pre-meal soluble human insulin in type 1 diabetes. Diabetes Res Clin Pract. 2005 Jul 26; [Epub ahead of print]
6. Home PD, Pocock SJ, Beck-Nielsen H, Gomis R, Hanefeld M, Dargie H, Komajda M, Gubb J, Biswas N, Jones NP. Rosiglitazone Evaluated for Cardiac Outcomes and Regulation of Glycaemia in Diabetes (RECORD): study design and protocol. Diabetologia. 2005 Sep;48(9):1726-35. Epub 2005 Jul 16.
7. Home PD, Rosskamp R, Forjanic-Klapproth J, Dressler A. A randomized multicentre trial of insulin glargine compared with NPH insulin in people with type 1 diabetes. Diabetes Metab Res Rev. 2005 Jul 15; [Epub ahead of print]
8. Jennings CE, Owen CJ, Wilson V, Pearce SHS. A haplotype of the CYP27B1 promoter is associated with autoimmune Addison’s disease but not with Graves’ disease in a UK population. J Mol Endo 2005; 34: 859-863.
9. MacColl G & Quinton R. 2005 Kallmann's syndrome: bridging the gaps. Journal of Paediatric Endocrinology & Metabolism. 18: 541-543.
10. Perros P. A 69-year-old female with tiredness and a persistent tan. PLoS Med. 2005 Aug;2(8):e229. Epub 2005 Aug 30.
11. Perros P, Kendall-Taylor P, Neoh C, Frewin S, Dickinson J. A prospective study of the effects of radioiodine therapy for hyperthyroidism in patients with minimally active graves' ophthalmopathy. J Clin Endocrinol Metab. 2005 Sep;90(9):5321-3. Epub 2005 Jun 28.
12. Putta-Manohar S, Syed AA, Parr JH. Cutaneous lesions on the legs. J Postgrad Med 2005; 51(2):127-30.
13. Quinton R & Brownrigg H. The Riots in Kandy. In: More Tales from the Travellers. Editor: Chris Bonnington, Martin Tomkinson Publications, 22 June 2005, ISBN: 0905500741.
14. Roglic G, Unwin N, Bennett PH, Mathers C, Tuomilehto J, Nag S, Connolly V, King H. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care. 2005 Sep;28(9):2130-5.
15. Sibal L, Ball SG, Connolly V, James RA, Kane P, Kelly WF, Kendall-Taylor P, Mathias D, Perros P, Quinton R, Vaidya B. Pituitary Apoplexy: A Review of Clinical Presentation, Management and Outcome in 45 Cases. Pituitary. 2005 Jul 11; [Epub ahead of print]
16. Sjolie AK, Porta M, Parving HH, Bilous R, Klein R; The DIRECT Programme Study Group. The DIabetic REtinopathy Candesartan Trials (DIRECT) Programme: baseline characteristics. J Renin Angiotensin Aldosterone Syst. 2005 Mar;6(1):25-32.
17. Syed AA, Weaver JU. Glucocorticoid sensitivity: the hypothalamic-pituitary-adrenal-tissue axis. Obes Res. 2005 Jul;13(7):1131-3.
18. Weaver JU. Obesity, cytokines and the search for beauty. Clin Endocrinol (Oxf). 2005 Sep;63(3):251-2.
19. Walker M, Taylor RW, Turnbull DM. Mitochondrial diabetes. Diabet Med. 2005 Sep;22 Suppl 4:18-20.
RECENT PUBLICATIONS IN DIABETES & ENDOCRINOLOGY THAT HIT THE NEWS OR THAT MAY HAVE A SIGNIFICANT IMPACT ON MANAGEMENT
Reid IR, Miller P, Lyles K, Fraser W, Brown JP, Saidi Y, Mesenbrink P, Su G, Pak J, Zelenakas K, Luchi M, Richardson P,Hosking D. Comparison of a single infusion of zoledronic acid with risedronate for Paget's disease. NEJM 2005;353:872-5.
Two identical, randomized, double-blind, actively controlled trials of 6 months' duration compared one 15-minute infusion of 5 mg of zoledronic acid with 60 days of oral risedronate (30 mg per day). The primary efficacy end point was the rate of therapeutic response at six months, defined as a normalisation of alkaline phosphatase levels or a reduction of at least 75% in the total alkaline phosphatase excess. The results of the studies were pooled. RESULTS: At six months, 96% of patients receiving zoledronic acid had a therapeutic response as compared with 74.3% of patients receiving risedronate (p less than 0.001). Alkaline phosphatase levels normalised in 88.6% of patients in the zoledronic acid group and 57.9% of patients in the risedronate group (p less than 0.001). Zoledronic acid was associated with a shorter median time to a first therapeutic response (64 vs. 89 days, p less than 0.001). Higher response rates in the zoledronic acid group were consistent across all demographic, disease-severity, and treatment-history subgroups and with changes in other bone-turnover markers. The physical-component summary score of the Medical Outcomes Study 36-item Short-Form General Health Survey, a measure of the quality of life, increased significantly from baseline at both three and six months in the zoledronic acid group and differed significantly from those in the risedronate group at 3-months. Pain scores improved in both groups. During post-trial follow-up (median, 190 days), 21 of 82 patients in the risedronate group had a loss of therapeutic response, as compared with 1 of 113 patients in the zoledronic acid group (p less than 0.001). In conclusion a single infusion of zoledronic acid produces more rapid, more complete, and more sustained responses in Paget's disease than does daily treatment with risedronate.
Cundy T, Davidson J, Rutland MD, Stewart C, DePaoli AM. Recombinant osteoprotegerin for juvenile Paget's disease. NEJM 2005;353:918-23.
Juvenile Paget's disease, a genetic bone disease characterized by accelerated bone turnover, results from inactivating mutations in the gene encoding osteoprotegerin--a key regulator of osteoclastogenesis. The effects of recombinant osteoprotegerin were investigated in two adult siblings with juvenile Paget's disease. Bone resorption (assessed by N-telopeptide excretion) was suppressed by once-weekly subcutaneous doses of 0.3 to 0.4 mg per kilogram of body weight. After 15 months of treatment, radial bone mass increased in one patient by 9 percent and in the other by 30 percent, skeletal bisphosphonate retention decreased by 37 percent and 55 percent, respectively, and there was radiographic improvement. Apart from mild hypocalcaemia and hypophosphataemia, no apparent adverse events occurred. Read the accompanying perspectives article by Deftos LJ, NEJM 2005;353:872-875, relating to these 2 articles. It is excellent.
Ehrmann DA. Polycystic Ovary Syndrome. NEJM 2005;352:1223-1236.
An excellent review article that is of practical and intellectual value.
Watanabe D, Suzuma K, Matsui S, Kurimoto M, Kiryu J, Kita M, Suzuma I, Ohashi H, Ojima T, Murakami T, Kobayashi T, Masuda S, Nagao M, Yoshimura N, Takagi H. Erythropoietin as a retinal angiogenic factor in proliferative diabetic retinopathy. NEJM 2005;353:782-92.
The investigators measured both erythropoietin and VEGF levels in the vitreous fluid of 144 patients with the use of radioimmunoassay and enzyme-linked immunosorbent assay. Vitreous proliferative potential was measured according to the growth of retinal endothelial cells in vitro and with soluble erythropoietin receptor. In addition, a murine model of ischemia-induced retinal neovascularization was used to evaluate erythropoietin expression and regulation in vivo. RESULTS: The median vitreous erythropoietin level in 73 patients with proliferative diabetic retinopathy was significantly higher than that in 71 patients without diabetes (464.0 vs. 36.5 mIU per milliliter, p less than 0.001). The median VEGF level in patients with retinopathy was also significantly higher than that in patients without diabetes (345.0 vs. 3.9 pg per milliliter, p less than 0.001). Multivariate logistic-regression analyses indicated that erythropoietin and VEGF were independently associated with proliferative diabetic retinopathy and that erythropoietin was more strongly associated with the presence of proliferative diabetic retinopathy than was VEGF. Erythropoietin and VEGF gene-expression levels are up-regulated in the murine ischaemic retina, and the blockade of erythropoietin inhibits retinal neovascularization in vivo and endothelial-cell proliferation in the vitreous of patients with diabetic retinopathy in vitro. This study suggests that erythropoietin is a potent ischemia-induced angiogenic factor that acts independently of VEGF during retinal angiogenesis in proliferative diabetic retinopathy. Any therapy that is in the pipeline relating to erythropoietin blockade is probably best delivered locally because of its uncertain systemic effects.
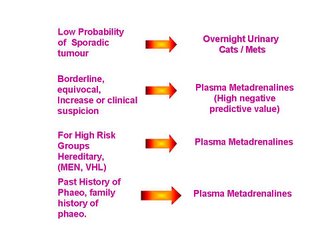
Lenders JWM, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet 2005;366:665-675. A review article that is a good revision aid.Matsumoto S, Okitsu T, Iwanaga Y, Noguchi H, Nagata H, Yonekawa Y, Yamada Y, Fukuda K, Tsukiyama K, Suzuki H, Kawasaki Y, Shimodaira M, Matsuoka K, Shibata T, Kasai Y, Maekawa T, Shapiro J, Tanaka K. Insulin independence after living-donor distal pancreatectomy and islet allotransplantation. Lancet 2005;365:1642-4.
Rising demand for islet transplantation will lead to severe donor shortage in the near future, especially in countries where cadaveric organ donation is scarce. The investigators undertook a successful transplantation of living-donor islets for unstable diabetes. The recipient was a 27-year-old woman who had had brittle, insulin-dependent diabetes mellitus for 12 years. The donor, who was a healthy 56-year-old woman and mother of the recipient, underwent a distal pancreatectomy. After isolation, 408 114 islet equivalents were transplanted immediately. The transplants functioned immediately and the recipient became insulin-independent 22 days after the operation. The donor had no complications and both women showed healthy glucose tolerance. Transplantation of living-donor islets from the distal pancreas can be sufficient to reverse brittle diabetes.
Feenstra J, de Herder WW, ten Have SM, van den Beld AW, Feelders RA, Janssen JA, van der Lely AJ. Combined therapy with somatostatin analogues and weekly pegvisomant in active acromegaly. Lancet 2005;365:1644-6.
Pegvisomant monotherapy once daily returns concentrations of insulin-like growthfactor I (IGF-I) to normal in most patients with acromegaly, but is very costly. In a 42-week dose-finding study, the investigators assessed the efficacy of the combination of long-acting somatostatin analogues once monthly and pegvisomant once weekly in 26 patients with active acromegaly. Dose of pegvisomant was increased until IGF-I concentration became normal or until a weekly dose of 80 mg was reached. IGF-I reached normal concentrations in 18 of 19 (95%) patients who completed 42 weeks of treatment, with a median weekly dose of 60 mg pegvisomant (range 40-80). No signs of pituitary tumour growth were noted, but mild increases in liver enzymes were observed in ten patients (38%). This combined treatment is effective, might increase compliance, and could greatly reduce the costs of medical treatment for acromegaly in some patients.
IDF First Global guidelines for management of type 2 diabetes
On 13th Sept at Athens the EASD congress the IDF release of the first global guidelines for the management of T2DM. The guidelines call for more aggressive treatment of type 2 diabetes across the globe with detailed 3 level care approach. For full version check www.idf.org
The metabolic syndrome: time for a critical appraisal.
An excellent review article from the joint statement of ADA and EASD published in Diabetes Care. 2005 Sep;28(9):2289-304. Definitely worth reading!!
Dahlof B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J; ASCOT Investigators. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366:895-906.
This multicentre, prospective, randomised controlled trial compare the effect on non-fatal MI and fatal CHD of combinations of atenolol with a thiazide versus amlodipine with perindopril in 19 257 patients with hypertension who were aged 40-79 years and had at least three other cardiovascular risk factors. Patients were assigned either amlodipine 5-10 mg adding perindopril 4-8 mg as required (amlodipine-based regimen; n=9639) or atenolol 50-100 mg adding bendroflumethiazide 1.25-2.5 mg and potassium as required (atenolol-based regimen; n=9618). The primary endpoint was non-fatal MI (including silent MI) and fatal CHD. Analysis was by intention to treat. The study was stopped prematurely after 5.5 years' median follow-up and accumulated in total 106 153 patient-years of observation. Though not significant, compared with the atenolol-based regimen, fewer individuals on the amlodipine-based regimen had a primary endpoint (429 vs 474; unadjusted HR 0.90, 95% CI 0.79-1.02, p=0.1052), fatal and non-fatal stroke (327 vs 422; 0.77, 0.66-0.89, p=0.0003), total cardiovascular events and procedures (1362 vs 1602; 0.84, 0.78-0.90, p less than 0.0001), and all-cause mortality (738 vs 820; 0.89, 0.81-0.99, p=0.025). The incidence of developing diabetes was less on the amlodipine-based regimen (567 vs 799; 0.70, 0.63-0.78, p less than 0.0001). In conclusion the amlodipine-based regimen prevented more major cardiovascular events and induced less diabetes than the atenolol-based regimen. The authors state that these results have implications with respect to optimum combinations of antihypertensive agents. From a personal point of view this trial does not change my own clinical practice of perindopril followed by bendrofluamethazide followed by amlodipine followed by doxazosin followed by atenolol when managing hypertension. This practice is certainly not written in stone and I do individualise treatment. ASCOT simply shows that there is little to choose between older and newer agents. The provocative accompanying editorial argues that the 2.7mmHg difference in systolic BP between the amlodipine/perindopril vs BFZ/atenolol arm can account for the difference between the regimens. A lot of marketing pressure is going to be applied to Drs over coming months in relation to the results of ASCOT. My advice will be to be consistent as advised by one of my trainers whilst I was towards the end of my training. If you prefer to use lisinopril or methyldopa stick to it, but strive to achieve target blood pressures. Even in ASCOT only 32.2% of diabetic and 60% of non-diabetic patients were well controlled.
Ashen MD, Blumenthal RS. Clinical practice. Low HDL cholesterol levels. N Engl J Med. 2005 Sep 22;353(12):1252-60.
This is an excellent review article which discusses the scientific basis behind lowering HDL and relates to clinical practice. A worthwhile read.
NEXT NEWSLETTER Due out beginning of February 2006, so keep the gossip coming.
NORTHEAST NEWSLETTER
FOR SPRs AND BOSSES TRAPPED IN THE NORTHERN DEANERY
October 2005
Editors: Shahid Wahid and Petros Perros
Associate Editors: Freda Razvi, Akheel Syed and Ebaa Al-Ozairi
SpR PLACEMENTS (NTN/VTN year of training from 1st October 2005)
RVI- Arun(5), Salman Razvi (3), Akheel Syed (4), Andrew Advani (3/4), Suresh Vaikkakara (visiting SpR)
Freeman- Eelin Lim(3), Reena Thomas (4), Vishmawitra Sharma
North Tyneside/Wansbeck- Muthu Jayapaul (3) /Chandima Idampitiya (1)
South Tyneside- Ibrahim M Ibrahim (4)
Gateshead- Ravi Erukalapati(1)
Sunderland-Isha Malik(1), Subir Ray (2)
North Tees/Hartlepool- Sony Anthony(4)/ Peter Carey(3)
Middlesbrough- Simon Ashwell(5), Sukesh Chandran (2), Asgar Madathil (2)
Carlisle- Khaled Mansur-Dukhan (2)
Bishop Auckland / Durham- Beas Bhatacharya (3)/Jeevan Metayil (1)
NGH/QEH- Yasir Elkhatim
Research with numbers (supervisor)- Latika Sibal (Prof Home), Arutchelvan Vijayaraman (Prof Home), Ravikumar Balasubramanian (Prof Taylor), Ebaa Al-Ozairi (USA-Prof Home)
Acting up David Woods (5)
MEETINGS / LECTURES / ANNOUNCEMENTS
10th-11th October 2005 Controversy or Consensus in the Diabetic Foot Conference, London. Contact SB Communications Group
21ST October 2005 Deadline for BES abstract submission. See www.ece2006.com
25th October 2005 55th Meeting of British Thyroid Association, London. Contact Mark Vanderpump
26th-27th October 2005 ABCD Autumn meeting, London. Contact www.diabetologists.org.uk
26thOctober 2005 Northern Endocrine & Diabetes Autumn CME,James Cook University Hospital. Contact Simon Ashwell .
3rd November 2005 RCP Update in Medicine, Freeman Hospital. Contact Lorraine Waugh
7th-9th November 2005 196th Meeting of the Society for Endocrinology, London. Contact www.endocrinology.org
9th November 2005 North East Obesity Forum, Freeman Hospital 1600-1800, “the Liver in Obesity”. Contact Karen Blackburn or Nigel Unwin
12th November 2005 Association of Physicians meeting,South Tyneside District Hospital. Contact Roy Taylor .
14th November 2005 Regional Neuroendocrine Tumour Meeting, Freeman Hospital 1730-2030, Contact Beverley Ashton
14th-16th November 2005 3rd National MED REG conference, London. Contact www.mahealthcareevents.co.uk or Mark Allen Group
25th November 2005 Abstract Deadline for DUK APC Birmingham March 2006.
30th November 2005 Northern Endocrine Regional Research and Audit Group (NERRAG) meeting, Lumley Castle, Chester-le-street, Durham. Contact Shahid Wahid
14th December 2005 GIM training ½ day-Freeman Hospital. Contact Lorraine Waugh 0191 223 1247 Lorraine Waugh
15th December 2005 SpR Assessment methods training workshop, James Cook University Hospital 1230-1700. Contact Helen Scales
15th February 2006 Society for Endocrinology Clinical Cases meeting, London. Contact Ann Lloyd
TRAINING ISSUES
Registering with JCHMT/PMETB It is essential that all new SpRs (even LATs) register with the PMETB (used to be JCHMT). Not doing so means your training is not counted and you cannot have a RITA.
SpR Feedback Recently feedback forms for training posts have been circulated to all SpRs. Please complete one form for each training post you have been to in the region as an SpR and return electronically to Shaz Wahid. The results for each individual unit will be sent to them along with a regional summary for comparison. This will allow individual units to improve training. The summary results and examples of practice will be discussed at the annual Trainers meeting. The process will be completed every 3-yrs (to coincide with planned Programme Director change over) so to maintain SpR anonymity.
SpR Database The STC are building an updated database of trainees. Could all SpRs with a number forward their NTN details and CCT date ASAP to Shaz Wahid.
Log Book/Portfolio Documentation It is a trainees responsibility to make sure their portfolio/log book is prospectively completed and the necessary signatures obtained. Any experience that is not signed off by your educational supervisor at the time cannot be counted towards training.
The Run Through Grade-An update from Shaz Wahid and John Parr As of August 2007 all SHO posts in the region “will” join the PIMD school of medicine, with Basic Specialist Training in Medicine provided in 2-year rotations based around 4 geographical areas with associated hospitals: Wearside (Sunderland Royal, South Tyneside); Newcastle (FRH, FRH, QEH, Northumbria); Durham (UHND, Bishop Auckland, Darlington); Teeside (JCUH, Friaridge, North Tees, Hartlepool). The rotations will be governed by the PIMD. Although floated in a discussion document initially, at a recent GIM STC meeting Nancy Redfern has confirmed that the deanery will be adapting this model. A lot of groundwork is required (an understatement) and the following preliminary timetable was sketched out for our region:
1. By Jan 06
All the "Ology" Specialty programme directors/committees will be consulted and asked what they want of the BST programme for people acceptable to their specialty training programmes, and how do they want to be represented; this will also include the likes of Radiology where medical SHOs also currently go to (the current estimate is that only 40% SHOs go onto medical specialty training programmes so other routes of specialization also need to be catered for in a Basic Medical Specialty Training Programme.
How many non-F2 SHOs (approved posts; Trust doctors; Clinical Fellows etc) do we have in the region?
What posts do we have within the "obvious base units" and are there enough posts to provide suitable rotations?
Who will be the local Trust doctor charged with doing the donkey work within each Trust?
Workforce Planning issues to be sorted out with SHA.
2. By March 06
A draft working plan/document to be produced and presented.
Trusts' Managers to be approached formally.
Final document/plan to be agreed.
3. Between April and Dec 06.
Appoint Programme Directors;
Produce Rotation Specifications; Means of Assessment etc
Assess individual posts to ensure they can provide what the rotations need - (?Trainers may need to produce their own portfolio!).
Means of appointment (?National or Regional); Employment issues - e.g. Trust or Regional Contracts etc.
4. Feb 07
Advertise Posts for appointment for 1st August 2007
There are many outstanding issues which the PIMD will need to take on board; for example;
a) Role of current Royal College approval visits
b) Role of MRCP if the SHOs get their CCST in Acute Medicine at the end of the 2 year BST programme (the inference here is they may even be eligible as a Consultant in Acute Medicine after only 4 years training!).
c) What becomes of the "slow" trainee - will a 3rd year be needed?
d) How will the needs of Radiology, Dermatology, Anaesthesia etc be accommodated within the BST programme.
The STC is considering the implications of the above for our Training Programme. The PIMD are already setting up work-shops to prepare STCs for the Run through grade
Academic SpR rotation The STC are developing a post for an SpR to fill who is academically inclined. The details are still embryonic, but the attributes of future applicants should be:
-Wants an academic (eg. University, not NHS) career
-Already has a good first research degree (MD/PhD)
-Has already a significant publication record (eg. 4 rated papers for
the purposes of research assessment exercise [IF>5], or close to this)
-Has clear and independent research plans that will lead to an
application for a Clinician-scientist fellowship post within 12 months
of starting
-Has strong backing both from an Academic supervisor and a second
Clinical supervisor
-Has already been successful in obtaining some independent research
grant support
Obviously this is a tall order, and the post won't always be filled. An Academic SpR post will be a significantly different experience to a regular SpR post and not just a bland alternate designation with the same training expectations and experiences. Watch this space!
Community Diabetes Training/exposure in this area should consist of the following:
-Attendance at GP diabetes Clinics in the community to view process of care
-Participation in educational activities involving primary care health professionals
-Interaction with local Diabetes UK patient groups
-Attendance at a Diabetes Clinical Network or other management activity involving primary and secondary care interaction
-Participation with Diabetes Specialist Nurses in the community, e.g. home visit
Evidence may comprise reflective accounts, case based discussions, minutes of meetings, programme of events or feedback forms. These are the minimum training standards. Trainees keen to pursue a career in Community Diabetes will need a different slant to their rotation (cv academic rotation), which will require more extensive exposure to community diabetes and SOLID management training. The STC may have to look at this issue in due course.
SpR adverts for NTNs/LATs New PIMD regulations mean that each specialty will be allowed only 2 advertisements per year for Numbers/LAT appointments. The adverts for DM/Endo will be scheduled for end of September (this year 24th September) and Middle of April (next year 14th April). We therefore will only have 2 appointment panels per year for SpRs with a limited window. This has major implications:
1. All SpRs wishing to undertake an out of programme experience (formal research/travel abroad/acting up) or leave the rotation in 2006 are to give Shaz Wahid notice of the exact dates of absence(in writing) by the 1st March 2006. This will then allow the appropriate advertisement to be placed in April 2006 with an appointments panel convened in May/June 2006. Be warned that once SpRs have gave formal notice and the interviews have taken place with a replacement appointed for the period of absence from the rotation there is no going back. Any SpR missing this deadline will not be allowed to come off the rotation until the next appointments panel in October/November 2006 can appoint a replacement.
2. For SpRs with CCSTs due in 2006, the appointments panel in May/June 2006 will automatically appoint a replacement to start 6-months after their CCST date. This may be sooner, if the CCST holder accrues a post earlier than their 6-month grace and enough notice has been given to the appointments panel.
Inevitably a gap may arise in the rotation. The PIMD will post an advert for a LAS that does not require an appointments panel.
New Assessment tools Please see the following website. As of October 2005 Multisource feedback (MSF) and Directly Observed Procedural Skills (DOPS) will be formally introduced and Mini Clinical Evaluation Exercise (Mini-CEX) will go live from October 2006. Also read Ebaa’s excellent thought provoking letter below.
Training Committee Committee Chair- Jola Weaver; Regional Speciality Advisor- Richard Quinton; Programme Director- Shahid Wahid; Consultant member- Jean Macleod; Consultant member (Research Advisor)-Simon Pearce; Consultant member- Simon Eaton; Consultant member- Ronan Canavan; SpR representative- Simon Ashwell; SpR representative- Andrew Advani.
NEW FACES ON THE SCENE
Welcome to Chandima Idampitiya. She joins us as a new NTN beginning at Northumbria.
Welcome to Suresh Vaikkakara. He is a visiting SpR from India based at the RVI.
OLD FACES ON THE GO
Congratulations to Kamal Abouglila on appointment to the post of Consultant in Diabetes and Endocrinology at University Hospital of North Durham.
NEWS FROM THE NORTHEAST
Congratulations to Jeevan Matayil and Ravi Erukulapati on their NTNs.
Congratulations to Richard Quinton and Family on the birth of Baby Oliver.
Congratulations to Akheel Syed and family on the birth of baby boy sunain.
The Programme Director Change has been brought forward, with Shaz Wahid taking over from Richard Quinton on 1st October 2005.
LETTERS
Contributions for this section can include meeting reports, research experiences, book reviews, experiences abroad, and anything else you feel may benefit trainees and trainers around the region. The success of this section really does depend on YOU.
The Death of General Medicine as a dual speciality is nigh
Shaz Wahid
Some may think I am mad, but throughout my training as both an SpR and SHO I thoroughly enjoyed GIM in both its acute medicine and out-patient varieties. My career choices have been coloured by Physicians such as David Carr, Rudy Bilous and Jean MacLeod to name but a few who have (had) established GIM out-patient clinics when I was on their team. This exposure I believe has contributed to my development. It was with a heavy heart that I have recently had to stop taking GIM out-patient referrals from GP colleagues and now run a mainly endocrine clinic with a spattering of ward follow-up patients. The reason for this is the ever-increasing specialist work-load and pressures such as choose and book to name a few. Once Acute Medicine becomes an entrenched speciality and there are enough Acute Physicians, even the acute medicine will disappear into the horizon and I will probably be writing a similar piece in ENDODIABOLOGY. What does this trend hold for future training programmes? I believe that the writing is on the wall for dual speciality training between GIM and DM&Endo. When this may occur is any ones guess, but the split may well be traumatic.
RCP Assessment Tools: Grading the Graders- The missing link!!!
Ebaa Al-ozairi
Assessment is an essential element of all educational systems and to be useful it must be viewed as an integral rather than series of events. Royal College of Physicians (RCP) has recently released new assessment tools for SpRs. Many of the tools have been widely used in the USA and Canada; however can they be applied to the UK system???? In my one year of experience in the USA at Harvard with the remodelling of postgraduate training in the UK has fuelled me to explore discrepancy in the training system and the impact towards a better training system
With the development of modernizing medical careers, it has come to my attention that the onus is on the trainee themselves including evaluation, continuing assessment and examination with huge issue not being addressed: GRADING THE GRADERS- The missing link!!!!!
Mini-Cex: While this method is certainly widely used in USA for the medical students it is hardly used at the fellow stages (equivalent to the SpR stage). Both the American Board of Internal medicine and the fellowship exams are solely based on MCQ with no clinical components. In Canada twice a year mini-cex evaluation takes place in the residency program to prepare the interns for the clinical component of internal medicine exams. Both USA and Canadian systems do not allow interns or fellows to see any in-patient consultation or outpatient without individual discussion of the plan in the presence of the attending (Consultant) who needs to see every single case both at the inpatient and the Outpatient and this is regarded as continuing educational process and mimic the Mini Cex for the later stages. This certainly can not be applied to UK training due to the number of patients seen.
MSF and Raters: I strongly believe in team work and the concept is very appealing. However this method may be useful as an assessment tool after foundation year and may be in the initial stages of higher training but certainly neither in the last 2 years when SpR should be looked at as a senior figure nor at foundation year 1 (F1). Why should doctors get assessed by the allied health professional when they are not assessed by SpR and junior doctors???? Junior doctors in the UK are under so much pressure by the nursing staff and in my opinion the majority of the house officers have enough stress at this stage.
In both the USA and the Canadian system an essential part of the assessment is the complete evaluation of the residents and fellows by their staff (consultant). This is a detailed evaluation of availability, patient care, teaching, communication skills and system based practice. I strongly believe this is a powerful tool that has been missed out at the postgraduate stage although it is widely emphasized in the UK undergraduate system
Similarly the attending evaluates the residents/fellow however it is the duty of the of the attending to take the lead in arranging the evaluation dates and discussing all the evaluations with the resident/fellow rather than resident/fellow running around making appointments.
I strongly believe in assessment as a tool to validate educational effort. Without adequate summative assessment we can not fulfil our obligation to society to assure physicians training meets the higher state of knowledge, competence and professionalism. The UK has been well known for the quality of trained physicians but the time came to polish up to excellence level.
RECENT PUBLICATIONS FROM THE NORTHEAST
Please send us your recent publication for inclusion in the next newsletter.
1. Brook, Clayton and Brown: Clinical Paediatric Endocrinology (5e), which will be launched this month at the European Society of Paediatric Endocrinology meeting with a chapter "Polyglandular Syndromes" by Owen CJ, Cheetham TD and Pearce SH.
2. Carey PE, Gerrard J, Cline GW, Dalla Man C, English PT, Firbank MJ, Cobelli C, Taylor R. ACUTE INHIBITION OF LIPOLYSIS DOES NOT AFFECT POST-PRANDIAL SUPPRESSION OFENDOGENOUS GLUCOSE PRODUCTION. Am J Physiol Endocrinol Metab. 2005 Jul 5; [Epub ahead of print]
3. Hart RH, Kendall-Taylor P, Crombie A, Perros P. Early response to intravenous glucocorticoids for severe thyroid-associated ophthalmopathy predicts treatment outcome. J Ocul Pharmacol Ther. 2005 Aug;21(4):328-36.
4. Home PD, Home EM. International textbook of diabetes mellitus. Diabet Med. 2005 Oct;22(10):1460.
5. Home PD, Hallgren P, Usadel KH, Sane T, Faber J, Grill V, Friberg HH. Pre-meal insulin aspart compared with pre-meal soluble human insulin in type 1 diabetes. Diabetes Res Clin Pract. 2005 Jul 26; [Epub ahead of print]
6. Home PD, Pocock SJ, Beck-Nielsen H, Gomis R, Hanefeld M, Dargie H, Komajda M, Gubb J, Biswas N, Jones NP. Rosiglitazone Evaluated for Cardiac Outcomes and Regulation of Glycaemia in Diabetes (RECORD): study design and protocol. Diabetologia. 2005 Sep;48(9):1726-35. Epub 2005 Jul 16.
7. Home PD, Rosskamp R, Forjanic-Klapproth J, Dressler A. A randomized multicentre trial of insulin glargine compared with NPH insulin in people with type 1 diabetes. Diabetes Metab Res Rev. 2005 Jul 15; [Epub ahead of print]
8. Jennings CE, Owen CJ, Wilson V, Pearce SHS. A haplotype of the CYP27B1 promoter is associated with autoimmune Addison’s disease but not with Graves’ disease in a UK population. J Mol Endo 2005; 34: 859-863.
9. MacColl G & Quinton R. 2005 Kallmann's syndrome: bridging the gaps. Journal of Paediatric Endocrinology & Metabolism. 18: 541-543.
10. Perros P. A 69-year-old female with tiredness and a persistent tan. PLoS Med. 2005 Aug;2(8):e229. Epub 2005 Aug 30.
11. Perros P, Kendall-Taylor P, Neoh C, Frewin S, Dickinson J. A prospective study of the effects of radioiodine therapy for hyperthyroidism in patients with minimally active graves' ophthalmopathy. J Clin Endocrinol Metab. 2005 Sep;90(9):5321-3. Epub 2005 Jun 28.
12. Putta-Manohar S, Syed AA, Parr JH. Cutaneous lesions on the legs. J Postgrad Med 2005; 51(2):127-30.
13. Quinton R & Brownrigg H. The Riots in Kandy. In: More Tales from the Travellers. Editor: Chris Bonnington, Martin Tomkinson Publications, 22 June 2005, ISBN: 0905500741.
14. Roglic G, Unwin N, Bennett PH, Mathers C, Tuomilehto J, Nag S, Connolly V, King H. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care. 2005 Sep;28(9):2130-5.
15. Sibal L, Ball SG, Connolly V, James RA, Kane P, Kelly WF, Kendall-Taylor P, Mathias D, Perros P, Quinton R, Vaidya B. Pituitary Apoplexy: A Review of Clinical Presentation, Management and Outcome in 45 Cases. Pituitary. 2005 Jul 11; [Epub ahead of print]
16. Sjolie AK, Porta M, Parving HH, Bilous R, Klein R; The DIRECT Programme Study Group. The DIabetic REtinopathy Candesartan Trials (DIRECT) Programme: baseline characteristics. J Renin Angiotensin Aldosterone Syst. 2005 Mar;6(1):25-32.
17. Syed AA, Weaver JU. Glucocorticoid sensitivity: the hypothalamic-pituitary-adrenal-tissue axis. Obes Res. 2005 Jul;13(7):1131-3.
18. Weaver JU. Obesity, cytokines and the search for beauty. Clin Endocrinol (Oxf). 2005 Sep;63(3):251-2.
19. Walker M, Taylor RW, Turnbull DM. Mitochondrial diabetes. Diabet Med. 2005 Sep;22 Suppl 4:18-20.
RECENT PUBLICATIONS IN DIABETES & ENDOCRINOLOGY THAT HIT THE NEWS OR THAT MAY HAVE A SIGNIFICANT IMPACT ON MANAGEMENT
Reid IR, Miller P, Lyles K, Fraser W, Brown JP, Saidi Y, Mesenbrink P, Su G, Pak J, Zelenakas K, Luchi M, Richardson P,Hosking D. Comparison of a single infusion of zoledronic acid with risedronate for Paget's disease. NEJM 2005;353:872-5.
Two identical, randomized, double-blind, actively controlled trials of 6 months' duration compared one 15-minute infusion of 5 mg of zoledronic acid with 60 days of oral risedronate (30 mg per day). The primary efficacy end point was the rate of therapeutic response at six months, defined as a normalisation of alkaline phosphatase levels or a reduction of at least 75% in the total alkaline phosphatase excess. The results of the studies were pooled. RESULTS: At six months, 96% of patients receiving zoledronic acid had a therapeutic response as compared with 74.3% of patients receiving risedronate (p less than 0.001). Alkaline phosphatase levels normalised in 88.6% of patients in the zoledronic acid group and 57.9% of patients in the risedronate group (p less than 0.001). Zoledronic acid was associated with a shorter median time to a first therapeutic response (64 vs. 89 days, p less than 0.001). Higher response rates in the zoledronic acid group were consistent across all demographic, disease-severity, and treatment-history subgroups and with changes in other bone-turnover markers. The physical-component summary score of the Medical Outcomes Study 36-item Short-Form General Health Survey, a measure of the quality of life, increased significantly from baseline at both three and six months in the zoledronic acid group and differed significantly from those in the risedronate group at 3-months. Pain scores improved in both groups. During post-trial follow-up (median, 190 days), 21 of 82 patients in the risedronate group had a loss of therapeutic response, as compared with 1 of 113 patients in the zoledronic acid group (p less than 0.001). In conclusion a single infusion of zoledronic acid produces more rapid, more complete, and more sustained responses in Paget's disease than does daily treatment with risedronate.
Cundy T, Davidson J, Rutland MD, Stewart C, DePaoli AM. Recombinant osteoprotegerin for juvenile Paget's disease. NEJM 2005;353:918-23.
Juvenile Paget's disease, a genetic bone disease characterized by accelerated bone turnover, results from inactivating mutations in the gene encoding osteoprotegerin--a key regulator of osteoclastogenesis. The effects of recombinant osteoprotegerin were investigated in two adult siblings with juvenile Paget's disease. Bone resorption (assessed by N-telopeptide excretion) was suppressed by once-weekly subcutaneous doses of 0.3 to 0.4 mg per kilogram of body weight. After 15 months of treatment, radial bone mass increased in one patient by 9 percent and in the other by 30 percent, skeletal bisphosphonate retention decreased by 37 percent and 55 percent, respectively, and there was radiographic improvement. Apart from mild hypocalcaemia and hypophosphataemia, no apparent adverse events occurred. Read the accompanying perspectives article by Deftos LJ, NEJM 2005;353:872-875, relating to these 2 articles. It is excellent.
Ehrmann DA. Polycystic Ovary Syndrome. NEJM 2005;352:1223-1236.
An excellent review article that is of practical and intellectual value.
Watanabe D, Suzuma K, Matsui S, Kurimoto M, Kiryu J, Kita M, Suzuma I, Ohashi H, Ojima T, Murakami T, Kobayashi T, Masuda S, Nagao M, Yoshimura N, Takagi H. Erythropoietin as a retinal angiogenic factor in proliferative diabetic retinopathy. NEJM 2005;353:782-92.
The investigators measured both erythropoietin and VEGF levels in the vitreous fluid of 144 patients with the use of radioimmunoassay and enzyme-linked immunosorbent assay. Vitreous proliferative potential was measured according to the growth of retinal endothelial cells in vitro and with soluble erythropoietin receptor. In addition, a murine model of ischemia-induced retinal neovascularization was used to evaluate erythropoietin expression and regulation in vivo. RESULTS: The median vitreous erythropoietin level in 73 patients with proliferative diabetic retinopathy was significantly higher than that in 71 patients without diabetes (464.0 vs. 36.5 mIU per milliliter, p less than 0.001). The median VEGF level in patients with retinopathy was also significantly higher than that in patients without diabetes (345.0 vs. 3.9 pg per milliliter, p less than 0.001). Multivariate logistic-regression analyses indicated that erythropoietin and VEGF were independently associated with proliferative diabetic retinopathy and that erythropoietin was more strongly associated with the presence of proliferative diabetic retinopathy than was VEGF. Erythropoietin and VEGF gene-expression levels are up-regulated in the murine ischaemic retina, and the blockade of erythropoietin inhibits retinal neovascularization in vivo and endothelial-cell proliferation in the vitreous of patients with diabetic retinopathy in vitro. This study suggests that erythropoietin is a potent ischemia-induced angiogenic factor that acts independently of VEGF during retinal angiogenesis in proliferative diabetic retinopathy. Any therapy that is in the pipeline relating to erythropoietin blockade is probably best delivered locally because of its uncertain systemic effects.
Lenders JWM, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet 2005;366:665-675. A review article that is a good revision aid.Matsumoto S, Okitsu T, Iwanaga Y, Noguchi H, Nagata H, Yonekawa Y, Yamada Y, Fukuda K, Tsukiyama K, Suzuki H, Kawasaki Y, Shimodaira M, Matsuoka K, Shibata T, Kasai Y, Maekawa T, Shapiro J, Tanaka K. Insulin independence after living-donor distal pancreatectomy and islet allotransplantation. Lancet 2005;365:1642-4.
Rising demand for islet transplantation will lead to severe donor shortage in the near future, especially in countries where cadaveric organ donation is scarce. The investigators undertook a successful transplantation of living-donor islets for unstable diabetes. The recipient was a 27-year-old woman who had had brittle, insulin-dependent diabetes mellitus for 12 years. The donor, who was a healthy 56-year-old woman and mother of the recipient, underwent a distal pancreatectomy. After isolation, 408 114 islet equivalents were transplanted immediately. The transplants functioned immediately and the recipient became insulin-independent 22 days after the operation. The donor had no complications and both women showed healthy glucose tolerance. Transplantation of living-donor islets from the distal pancreas can be sufficient to reverse brittle diabetes.
Feenstra J, de Herder WW, ten Have SM, van den Beld AW, Feelders RA, Janssen JA, van der Lely AJ. Combined therapy with somatostatin analogues and weekly pegvisomant in active acromegaly. Lancet 2005;365:1644-6.
Pegvisomant monotherapy once daily returns concentrations of insulin-like growthfactor I (IGF-I) to normal in most patients with acromegaly, but is very costly. In a 42-week dose-finding study, the investigators assessed the efficacy of the combination of long-acting somatostatin analogues once monthly and pegvisomant once weekly in 26 patients with active acromegaly. Dose of pegvisomant was increased until IGF-I concentration became normal or until a weekly dose of 80 mg was reached. IGF-I reached normal concentrations in 18 of 19 (95%) patients who completed 42 weeks of treatment, with a median weekly dose of 60 mg pegvisomant (range 40-80). No signs of pituitary tumour growth were noted, but mild increases in liver enzymes were observed in ten patients (38%). This combined treatment is effective, might increase compliance, and could greatly reduce the costs of medical treatment for acromegaly in some patients.
IDF First Global guidelines for management of type 2 diabetes
On 13th Sept at Athens the EASD congress the IDF release of the first global guidelines for the management of T2DM. The guidelines call for more aggressive treatment of type 2 diabetes across the globe with detailed 3 level care approach. For full version check www.idf.org
The metabolic syndrome: time for a critical appraisal.
An excellent review article from the joint statement of ADA and EASD published in Diabetes Care. 2005 Sep;28(9):2289-304. Definitely worth reading!!
Dahlof B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J; ASCOT Investigators. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366:895-906.
This multicentre, prospective, randomised controlled trial compare the effect on non-fatal MI and fatal CHD of combinations of atenolol with a thiazide versus amlodipine with perindopril in 19 257 patients with hypertension who were aged 40-79 years and had at least three other cardiovascular risk factors. Patients were assigned either amlodipine 5-10 mg adding perindopril 4-8 mg as required (amlodipine-based regimen; n=9639) or atenolol 50-100 mg adding bendroflumethiazide 1.25-2.5 mg and potassium as required (atenolol-based regimen; n=9618). The primary endpoint was non-fatal MI (including silent MI) and fatal CHD. Analysis was by intention to treat. The study was stopped prematurely after 5.5 years' median follow-up and accumulated in total 106 153 patient-years of observation. Though not significant, compared with the atenolol-based regimen, fewer individuals on the amlodipine-based regimen had a primary endpoint (429 vs 474; unadjusted HR 0.90, 95% CI 0.79-1.02, p=0.1052), fatal and non-fatal stroke (327 vs 422; 0.77, 0.66-0.89, p=0.0003), total cardiovascular events and procedures (1362 vs 1602; 0.84, 0.78-0.90, p less than 0.0001), and all-cause mortality (738 vs 820; 0.89, 0.81-0.99, p=0.025). The incidence of developing diabetes was less on the amlodipine-based regimen (567 vs 799; 0.70, 0.63-0.78, p less than 0.0001). In conclusion the amlodipine-based regimen prevented more major cardiovascular events and induced less diabetes than the atenolol-based regimen. The authors state that these results have implications with respect to optimum combinations of antihypertensive agents. From a personal point of view this trial does not change my own clinical practice of perindopril followed by bendrofluamethazide followed by amlodipine followed by doxazosin followed by atenolol when managing hypertension. This practice is certainly not written in stone and I do individualise treatment. ASCOT simply shows that there is little to choose between older and newer agents. The provocative accompanying editorial argues that the 2.7mmHg difference in systolic BP between the amlodipine/perindopril vs BFZ/atenolol arm can account for the difference between the regimens. A lot of marketing pressure is going to be applied to Drs over coming months in relation to the results of ASCOT. My advice will be to be consistent as advised by one of my trainers whilst I was towards the end of my training. If you prefer to use lisinopril or methyldopa stick to it, but strive to achieve target blood pressures. Even in ASCOT only 32.2% of diabetic and 60% of non-diabetic patients were well controlled.
Ashen MD, Blumenthal RS. Clinical practice. Low HDL cholesterol levels. N Engl J Med. 2005 Sep 22;353(12):1252-60.
This is an excellent review article which discusses the scientific basis behind lowering HDL and relates to clinical practice. A worthwhile read.
NEXT NEWSLETTER Due out beginning of February 2006, so keep the gossip coming.